Mayo Clinic researchers combine form and function to drive holistic facial plastic surgery and reconstruction care.
Facial Plastic and Reconstructive Surgery
The Mayo Clinic Department of Otolaryngology — Head and Neck Surgery's Division of Facial Plastic and Reconstructive Surgery investigates clinically translatable predictive models, tissue biomechanics and patient-reported quality-of-life outcomes.
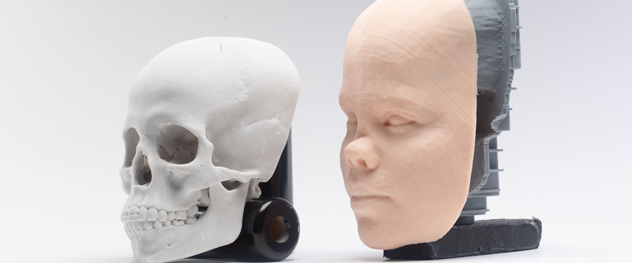
Investigators have partnered with Mayo's 3D Anatomic Modeling Laboratories to create 1-to-1 surgical models for preoperative planning and custom prosthetics for nonsurgical treatment of septal perforations. The division is also applying visual eye tracking software to better understand the impact of location, color and orientation of facial defects on viewer perception.
Predictive models
Anticipating patient satisfaction before surgery begins
Facial plastic surgery is a unique specialty in the field of otolaryngology in that a good outcome is defined by mutual agreement between the patient and surgeon before surgery. A predictive model to help clarify which patients are more or less likely to be satisfied with surgery is a valuable tool for increasing patient and surgeon satisfaction.
The Division of Facial Plastic and Reconstructive Surgery has published peer-reviewed research showing that preexisting personality traits and psychiatric diagnoses are unrelated to patient satisfaction. By using a validated consumer decision-making tool, researchers showed — for the first time — that their model can predict postoperative satisfaction.
Related publications:
Rhinoplasty planning
Rhinoplasty is considered by many clinicians to be the most challenging operation in facial plastic surgery, partially due to the variable thickness of the soft tissue of the nose, which is irregularly distorted during surgery by edema and local anesthesia.
Using CT scans, researchers in the Division of Facial Plastic and Reconstructive Surgery have developed normative data for the thickness of the nasal soft tissue envelope at various anatomical sites and have shown that experts in nasal analysis can reliably predict soft tissue thickness from photographs only.
Related publication:
3D anatomical modeling
3D printing
The Division of Facial Plastic and Reconstructive Surgery has worked closely with 3D-printing teams in the Mayo Clinic Department of Radiology and with Mayo Clinic prosthodontics specialists to develop unique 3D-printed models. These models can be used both for preoperative planning and for creating custom septal prosthetics to repair septal perforations that are unlikely to be closed with conventional surgical methods. Mayo Clinic is unique in offering these 3D-printed models to patients.
Related publication:
3D modeling
Septoplasty is one of the three most common operations in the head and neck. Unfortunately, the literature reports failure or revision rates of up to 15%.
To address this issue, Mayo Clinic facial plastic surgery researchers have investigated the biomechanical properties of the nasal septum by creating a computer model based on micro-CT scans of anatomical specimens. Using finite element modeling, the division has identified a more mechanically stable surgical structure for the septum. This new surgical structure has the potential to fundamentally change the way the operation is done.
Next steps are to perform a similar analysis of nasal tip cartilages to better understand their biomechanical properties. This may now be possible — for the first time — due to more-advanced imaging technology.
Eye tracking
Eye tracking technology is a helpful investigative tool for determining the relative impact and importance of various facial defects. Using eye tracking, it is possible to measure how distracting a skin cancer defect or a nasal deformity actually is. Studies are in progress to investigate clinical implications of this technology.