Research Focus
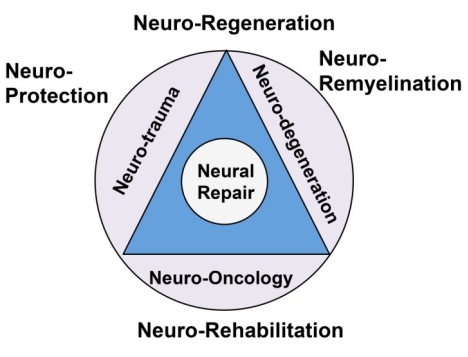
Summary of research directions in Dr. Scarisbrick's Neuroregeneration and Neurorehabilitation Laboratory.
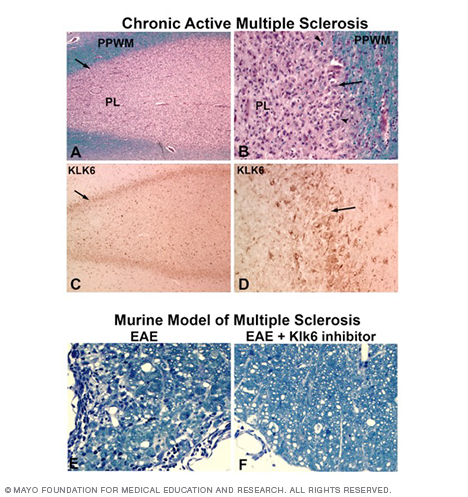
Dr. Scarisbrick's team discovered a novel secreted enzyme, kallikrein 6 (KLK6), that is highly elevated at sites of demyelination in multiple sclerosis (Scarisbrick et al., 2002). The enzyme works in part by degrading myelin directly and in part by directing pathogenic cellular activities by activating PAR1. Neutralization of this enzyme reduces inflammation and loss of myelin in inflammatory models of multiple sclerosis as cited in FASEB Journal, 2004 (Blaber et al.).
Dr. Scarisbrick's Neuroregeneration and Neurorehabilitation Laboratory at Mayo Clinic is identifying new regenerative and rehabilitative approaches for disorders of the central nervous system with particular emphasis on demyelinating conditions and trauma affecting the spinal cord. Spinal cord damage is a leading cause of disability. More than 1.5 million Americans have a spinal cord injury due to trauma, vascular injury, multiple sclerosis, oncogenesis or other causes.
There is significant opportunity for pharmacological, cellular and neuromodulatory interventions to improve functional outcomes for patients with brain and spinal cord injuries. As such, Dr. Scarisbrick's laboratory research team seeks to identify cellular and molecular mechanisms contributing to injury and repair processes in the spinal cord as therapeutic targets to improve neurological recovery.
To accomplish this, the lab is investigating factors that drive spinal cord pathogenesis across the life span, including inflammation, demyelination, axon injury and neuron degeneration. In addition, the lab is identifying factors that contribute to a lack of innate repair, including axon sprouting/regeneration, remyelination and rejuvenation by endogenous stem cells, and factors with the potential to limit or enhance emerging stem cell therapies and neuromodulatory interventions.
The long-range focus is to determine how combined approaches, including pharmacological, cellular and functional interventions, can be applied at appropriate time points to prevent pathogenesis and to promote plasticity and repair that will result in significant improvements in functional outcomes in patients with brain and spinal cord injuries.
Dr. Scarisbrick's Neuroregeneration and Neurorehabilitation Laboratory research team utilizes pharmacological approaches and genetically altered mice to study the roles of protease-activated receptors (PARs), metabolic dysfunction and exercise training in regulating nervous system physiology and response to injury. The lab has particular interests in studying signal transduction, neuron plasticity, astrogliosis and myelination. In vivo models are complemented by use of primary neuron and glial cell cultures, in addition to organotypic slice cultures to study underlying cellular mechanisms. Several new mouse models are being developed in the laboratory to uncover the effects of PARs and insulin signaling in the context of neural injury and repair.
To achieve these goals, Dr. Scarisbrick's lab has developed experimental spinal cord injury model systems that span the domains of trauma, ischemia, inflammatory demyelination and oncogenesis and is currently using these to determine common and potentially distinct molecular mechanisms of injury and repair in each setting. The lab's approach is further enhanced by pairing experimental models with the study of human materials to validate key findings and to identify therapeutic targets for rapid clinical translation.
Dr. Scarisbrick's lab identified select secreted serine proteases and the G-protein coupled receptors that activate protease-activated receptors (PARs) as highly druggable targets for pharmacotherapy with the potential to modulate the response of the spinal cord to injury and its capacity for innate repair and plasticity alone, or in response to rehabilitation. Ultimately, the preclinical findings obtained from these converging lines of investigation will form the basis for clinical trials to promote neuroprotection, neuroregeneration, neuroremyelination and neurorehabilitation to improve functional outcomes in patients with multiple sclerosis, spinal cord injuries or other neurological conditions.