 Overcoming transplant barriers
Overcoming transplant barriers
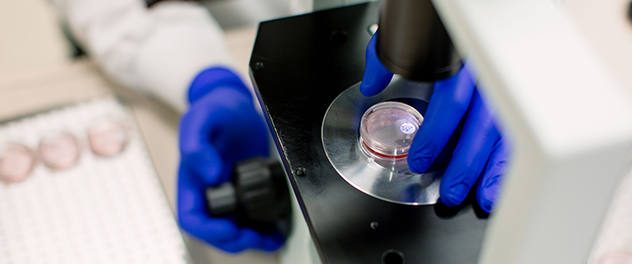
Using transplant immunology, regenerative medicine and tissue engineering applications, our lab is developing replacement tissues and organs for people with cardiovascular disease.
Overview
The Cardiovascular Tissue Engineering Research Laboratory helps people with cardiovascular disease through the sound application of transplant immunology, regenerative medicine and tissue engineering.
The lab, led by principal investigator Leigh G. Griffiths, Ph.D., MRCVS, at Mayo Clinic in Rochester, Minnesota, is dedicated to rigorous scientific investigation of cardiovascular disease.
Improving patient care
Our research is inspired by the devastating nature of cardiovascular disease and the increasing need for replacement organs and tissues. The need is especially pronounced in cardiovascular structures, where even minor tissue or organ dysfunction can precipitate catastrophic failure.
In addition, the parameters under which cardiovascular structures function are extremely arduous. The combination of exacting functional parameters and intolerance to even minor levels of dysfunction form the critical design criteria for attempts to produce replacement cardiovascular tissues or organs through tissue engineering.
Although this work inevitably involves bench-top scientific research, our lab team has a strong clinical foundation that drives judicious translation of its research discoveries into improved patient care.
Identifying biomarkers for rejection
Our transplant immunology work focuses on defining the barriers to human-to-human (allogeneic) and animal-to-human (xenogeneic) transplantation.
Under the expertise of Dr. Griffiths, the Cardiovascular Tissue Engineering Research Lab pioneered novel antigen identification technologies, allowing our research team to evaluate human leukocyte antigens (HLA, or their animal equivalents), non-HLA antigens (minor histocompatibility antigens) and nonprotein antigens (such as carbohydrates) longitudinally in individual transplant recipients.
Our goals are to identify preoperative and postoperative biomarkers for transplant rejection and thereby guide individualized therapy for transplant recipients.
Improving xenogeneic scaffolds
Many researchers are investigating methods of using animal tissues as tissue engineering scaffolds for development of tissue-engineered organs and tissues. When combined with a person's own cells, such scaffolds are capable of directing cell growth to build anatomically correct and functional tissues or organs.
While this approach shows great promise, unfixed animal-derived scaffolds contain components (antigens) that stimulate an aggressive immune rejection response after implantation.
Removal of antigenic components from the material before cell seeding and implantation in the patient represents a critical barrier to the use of animal-derived tissue scaffolds in tissue engineering and regenerative medicine applications.
We are working to apply a multidisciplinary approach to the development of ideal xenogeneic scaffolds for tissue engineering and regenerative medicine applications. Current research is directed at investigating the immune response to both allograft and xenograft tissues and organs.
Our lab team is using the knowledge gained through this work to develop new and more-effective methods of rendering xenogeneic scaffolds inert and thus tolerable to the immune system.
The scaffolds are then repopulated with cells, creating fully engineered tissues and organs that can be transplanted safely.