Overview
Vitiligo (vit-ih-LIE-go) is a disease that causes loss of skin color in patches. The discolored areas usually get bigger with time. The condition can affect the skin on any part of the body. It can also affect hair and the inside of the mouth.
Normally, the color of hair and skin is determined by melanin. Vitiligo occurs when cells that produce melanin die or stop functioning. Vitiligo affects people of all skin types, but it may be more noticeable in people with brown or Black skin. The condition is not life-threatening or contagious. It can be stressful or make you feel bad about yourself.
Treatment for vitiligo may restore color to the affected skin. But it doesn't prevent continued loss of skin color or a recurrence.
Products & Services
Symptoms
Vitiligo signs include:
- Patchy loss of skin color, which usually first appears on the hands, face, and areas around body openings and the genitals
- Premature whitening or graying of the hair on your scalp, eyelashes, eyebrows or beard
- Loss of color in the tissues that line the inside of the mouth and nose (mucous membranes)
Vitiligo can start at any age, but usually appears before age 30.
Depending on the type of vitiligo you have, it may affect:
- Nearly all skin surfaces. With this type, called universal vitiligo, the discoloration affects nearly all skin surfaces.
- Many parts of the body. With this most common type, called generalized vitiligo, the discolored patches often progress similarly on corresponding body parts (symmetrically).
- Only one side or part of the body. This type, called segmental vitiligo, tends to occur at a younger age, progress for a year or two, then stop.
- One or only a few areas of the body. This type is called localized (focal) vitiligo.
- The face and hands. With this type, called acrofacial vitiligo, the affected skin is on the face and hands, and around body openings, such as the eyes, nose and ears.
It's difficult to predict how this disease will progress. Sometimes the patches stop forming without treatment. In most cases, pigment loss spreads and eventually involves most of the skin. Occasionally, the skin gets its color back.
When to see a doctor
See your health care provider if areas of your skin, hair or mucous membranes lose coloring. Vitiligo has no cure. But treatment might stop or slow the discoloring process and return some color to your skin.
Causes
Skin layers and melanin
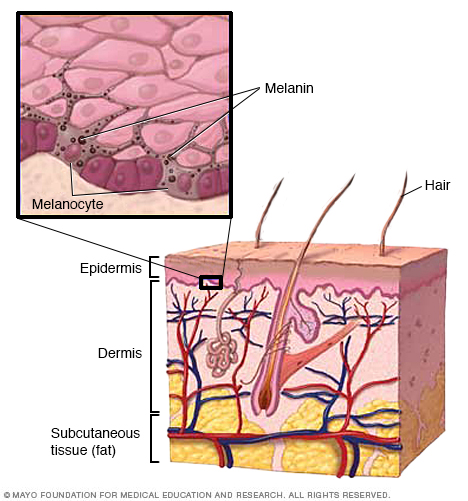
Skin layers and melanin
Melanin is a natural pigment that gives your skin its color. It's produced in cells called melanocytes.
Vitiligo occurs when pigment-producing cells (melanocytes) die or stop producing melanin — the pigment that gives your skin, hair and eyes color. The involved patches of skin become lighter or white. It's unclear exactly what causes these pigment cells to fail or die. It may be related to:
- A disorder of the immune system (autoimmune condition)
- Family history (heredity)
- A trigger event, such as stress, severe sunburn or skin trauma, such as contact with a chemical
Complications
People with vitiligo may be at increased risk of:
- Social or psychological distress
- Sunburn
- Eye problems
- Hearing loss
Nov. 10, 2022
- AskMayoExpert. Vitiligo. Mayo Clinic; 2019.
- Grimes PE. Vitiligo: Management and prognosis. https://www.uptodate.com/contents/search. Accessed Dec. 23, 2019.
- Grimes PE. Vitiligo: Pathogenesis, clinical features, and diagnosis. https://www.uptodate.com/contents/search. Accessed Dec. 23, 2019.
- Lebwohl MG, et al. Vitiligo. In: Treatment of Skin Disease: Comprehensive Therapeutic Strategies. 5th ed. Elsevier; 2018. https://www.clinicalkey.com. Accessed Dec. 23, 2019.
- Felsten LM, et al. Vitiligo: A comprehensive overview. Journal of the American Academy of Dermatology. 2011; doi:10.1016/j.jaad.2010.10.043.
- Whitton ME, et al. Interventions for vitiligo (review). Cochrane Database of Systematic Reviews. http://www.thecochranelibrary.com/view/0/index.html for link to abstract online. Accessed Dec. 23, 2019.
- Bae JM, et al. Phototherapy for vitiligo: A systematic review and meta-analysis. JAMA Dermatology. 2017; doi:10.1001/jamadermatology.2017.0002.
- Lee JH, et al. Treatment outcomes of topical calcineurin inhibitor therapy for patients with vitiligo: A systematic review and meta-analysis. JAMA Dermatology. 2019; doi:10.1001/jamadermatol.2019.0696.
- Thakur V, et al. Efficacy of transplantation of combination of noncultured dermal and epidermal cell suspension vs epidermal ell suspension alone in vitiligo: A randomized clinical trial. 2019; doi:10.1001/jamadermatol.2018.4919.
- Vitiligo. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/vitiligo. Accessed Dec. 23, 2019.
- Patient education: Vitiligo (The basics). https://www.uptodate.com/contents/search. Accessed Dec. 30, 2019.
- Vitiligo: Tips for managing. American Academy of Dermatology. https://www.aad.org/diseases/a-z/vitiligo-self-care. Accessed Dec. 30, 2019.
- Gibson LE (expert opinion). Mayo Clinic. Jan. 20, 2020.
Related
Products & Services